August 2023
How Peripheral Artery Disease Can Affect the Feet
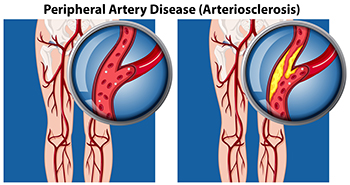
Peripheral artery disease, abbreviated PAD, also referred to as peripheral vascular disease, is a condition that arises from the reduced flow of blood to the body’s extremities, including the lower legs and feet. People with diabetes are more susceptible to developing PAD, as a result of weakened and damaged blood vessels from having high blood sugar. Blood clot formation within the vessels can also contribute to this condition. Conditions such as arthritis, which causes inflammation of the arteries, can further fuel peripheral artery disease. Other factors, such as smoking, hypertension, and obesity, increase the risk of developing PAD. Symptoms can include intermittent pain, coldness, numbness, and a bluish hue in the skin. In more advanced stages, wounds that resist healing, and areas of skin that blacken may develop due to the lack of adequate blood flow. In such cases, swift medical intervention is extremely important. If you suspect you may have peripheral artery disease that is affecting your lower extremities, it is suggested that you make an appointment with a podiatrist, who is specifically trained to manage this condition.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Brian D. Jackson, DPM from Neuhaus Foot and Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact one of our offices located in Columbia and Pulaski, TN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Rheumatoid Arthritis in Feet and Ankles

When rheumatoid arthritis, RA, targets the feet and ankles, life can feel unsteady. Foot and ankle arthritis not only brings pain but also disrupts balance and movement, making tasks like standing and walking difficult. Experts say 90% of RA patients experience foot or ankle pain, a rate twice that of the general population and primarily affecting women under 60. RA's impact is profound, and crippling foot pain can curtail daily activities. Symptoms of RA in the feet include swelling, stiffness, and deformities. Common issues include painful nodules, dislocated toe joints, bunions, and Achilles tendon pain. RA can strike the forefoot, midfoot, hindfoot, and ankle, altering mobility and causing distressing discomfort. While there is no cure for rheumatoid arthritis, various treatments alleviate RA-related foot pain. Strategies include gentle exercises, ice application, orthotics, braces, and accommodating shoes. Other measures include physical therapy, steroid injections, and surgical procedures. Surgery is a last resort and ranges from joint fusion to a replacement, each with unique risks and benefits. If you are suffering from rheumatoid arthritis that is affecting your feet, it is suggested that you make an appointment with a podiatrist.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Brian D. Jackson, DPM from Neuhaus Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact one of our offices located in Columbia and Pulaski, TN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Care for Your Arthritic Foot
Arthritis is an inflammation of the joints and it can occur at any joint in the body, especially in the foot. It generally effects those who are older, however, it can occur at any age. Although there are many different forms of arthritis, there are three main types that occur in the foot. The three types are osteoarthritis, rheumatoid arthritis, and gout.
The primary cause of osteoarthritis is aging. As you age, cartilage degenerates around the joints which causes friction and pain. Obesity can cause osteoarthritis through mechanical stress. Injuries that damage joints can increase the probability as well. Finally, a family history of osteoarthritis can also increase chances of having it.
Rheumatoid arthritis occurs when the immune system attacks the joint linings and weakens them over a long time. While there is no known cause of rheumatoid arthritis, obesity and smoking can increase your chances of getting it. Women are also more likely to get it than men.
Gout is a form of arthritis that occurs when there is too much uric acid in your blood and painful crystals form in your joints. Men are more likely to have gout than women. People who are obese or drink alcohol often are also more likely to develop gout. Furthermore, having diabetes, heart disease, high blood pressure, high cholesterol, gastric bypass surgery or a family history of gout may increase your likelihood of developing the condition.
Symptoms of arthritis include pain, stiffness, swelling in the joints. These symptoms can make it harder and more painful to walk. Physical activity can increase pain and discomfort. Furthermore, joint pain can worsen throughout the day for osteoarthritis. Gout attacks generally last several days with the first few being the worst.
Diagnosis of gout includes either a joint fluid test or a blood test. X-ray imaging can detect osteoarthritis but not gout. On the other hand, there is no blood test for osteoarthritis. Rheumatoid arthritis is difficult to diagnosis. Doctors utilize family and personal medical history, a physical examination, and antibody blood tests to determine if you have rheumatoid arthritis.
Treatment varies for the different kinds of arthritis. Anti-inflammatory medication or steroids can help reduce pain from inflammation of the joints. Changing shoe types can help with some symptoms. Wider shoes can help with discomfort from gout and osteoarthritis. High heels should be avoided. Shoes with proper arch support and that take pressure off the ball of the foot can help with rheumatoid arthritis. Drinking lots of water can also help rid uric acid from the blood. Losing weight, improving your diet, and limiting alcohol and smoking can also help prevent or lessen the symptoms of arthritis.
If you are having trouble walking or pain in your feet, see a podiatrist to check if you have arthritis.
Types and Locations of Ankle Sprains

Ankle sprains are common injuries that can occur during various physical activities. Ankle sprains are categorized into three degrees based on the severity of the ligament damage. A first-degree ankle sprain is mild, with stretched ligaments and minimal fiber damage. A second-degree sprain is more moderate, involving partially torn ligaments. The most severe type is a third-degree sprain, where ligaments are completely torn. Two main types of sprains are inversion and eversion. Inversion sprains occur when the foot twists inward, stretching the outer ligaments and causing pain on the outside of the ankle. Eversion sprains occur when the foot twists outward, stretching the inner ligaments and causing pain on the inside of the ankle. Ankle sprains can also also be classified based on their location. Lateral sprains occur on the outside of the ankle and makeup about 80 percent of all sprains. High, or syndesmotic, ankle sprains are rarer, seen in around 15 percent of ankle sprains. Medial sprains account for about 5 percent of all ankle sprains. Treatment for ankle sprains varies depending on the severity and location. It is suggested that you make an appointment with a podiatrist for a proper diagnosis and personalized treatment plan.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact Brian D. Jackson, DPM from Neuhaus Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact one of our offices located in Columbia and Pulaski, TN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Three Grades of Ankle Sprains
An ankle sprain occurs when one or more ankle ligament gets overly stretched. Ligaments are strong bands of tissue that bind and support the bones and other structures that make up the ankle. In more severe ankle sprains, the ligament(s) tear—either partially or completely—and there may be an audible popping noise at the moment of injury.
Ankle sprains are quite common and can occur when the ankle rolls outwardly (eversion) or inwardly (inversion), causing the ligament(s) to stretch beyond normal limits, or even tear. Falls, twists, or blows to the ankle during sports or other activities can cause this injury, as well as wearing improper footwear, running on uneven surfaces, or having weak ankles.
Depending on the injury’s severity, an ankle sprain will be classified as Grade I, Grade II, or Grade III. Grade I sprains involve ligament(s) being overly stretched but not torn, with symptoms of mild pain, swelling, and ankle instability. There may also be some difficulty bearing weight. A Grade II sprain usually involves a partial tear of the ligament which brings more intensity in these symptoms, along with possible bruising. With a Grade III sprain, the ligament is completely torn, the symptoms are severe, and it may not be possible to put weight on the affected foot at all.
To diagnose and grade an ankle sprain, a podiatrist will perform a physical examination, checking for tenderness and range of motion in the ankle. For more severe sprains, X-rays or other imaging studies may be necessary.
It is vitally important to have an ankle sprain treated properly as improper healing often leads to future ankle sprains and possibly even chronic ankle stability. Treatment for an ankle sprain will vary, depending on its severity, and may include the RICE method (Rest/Ice/Compression/Elevation), physical therapy, bracing, medications, and possibly even surgery to repair a torn ligament. Rehabilitation is very important for the sprain to heal properly and to restore functionality.
Definition and Causes of Achilles Tendon Injuries
The world of Achilles tendon injuries is common among athletes across the globe. The Achilles tendon is the band of tissue connecting the calf muscles to the heel bone, enabling us to walk, jump, and run. Achilles tendon injuries are described as tears or strains that happen to this crucial tendon. These injuries can be mild, causing discomfort, or severe pain, possibly causing difficulty in walking. A common cause of an Achilles tendon injury can be from overuse. This can range from increasing speed and mileage too quickly while running to not getting adequate rest. Wearing improper footwear, such as flip-flops during sporting activities, can also contribute to this painful condition. Additionally, sudden increases in physical activity or tight calf muscles may put stress on the Achilles tendon, leading to injuries. Effective prevention techniques can include stretching, wearing suitable shoes, and listening to your body's limits. If you have endured this type of injury, it is suggested that you visit a podiatrist sooner rather than later who can provide you with relief solutions.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Brian D. Jackson, DPM of Neuhaus Foot and Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Columbia and Pulaski, TN . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
The Causes, Types, and Treatments of Achilles Tendon Injuries
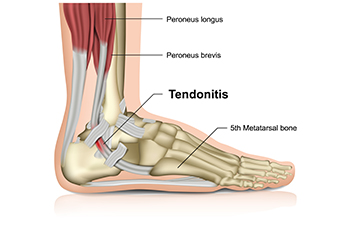
Tendons are fibrous tissues that connect muscles with bone. The Achilles tendon is the largest tendon in the body. It connects the calf muscles at the back of the leg with the heel, and facilitates movements such as jumping, running, and walking.
Because the Achilles tendon is engaged so frequently and bears a great deal of pressure and stress throughout the day, it can become injured. Achilles tendon injuries cause the tissue to become irritated, inflamed, and swollen. Pain can come on gradually or be immediate, and will vary from mild to severe depending upon the injury. Where the pain occurs will vary as well, from just above the heel up through the back of the leg. There may also be stiffness in the tendon.
Achilles tendon injuries can often be caused by repetitive stress. They may also occur while running, playing tennis, gymnastics, football, basketball, dancing, soccer, baseball or other sports that require speeding up, slowing down, or pivoting quickly. Wearing high heels, falling from an elevation, stepping in a hole, having flat feet, bone spurs, tight leg muscles or tendons, wearing improper athletic shoes, exercising on uneven surfaces, or starting a new type of exercise can also cause Achilles tendon injuries.
The two most common Achilles tendon injuries are tendonitis and ruptures. Tendonitis causes painful inflammation and can occur in different parts of the tendon. Non-insertional Achilles tendonitis occurs when the fibers in middle of the tendon begin to break down, thicken, and swell. This condition typically affects younger, more active adults. Insertional Achilles tendonitis occurs where the tendon inserts into the heel bone. It is common for bone spurs to form with this type of injury. This condition can affect people of any age and level of activity.
Achilles tendon ruptures are a tear in the tendon. These breaks may be partial or complete. There may be an audible popping noise at the moment of injury and the pain will be sudden and severe.
An Achilles tendon injury can be diagnosed by your podiatrist after they examine you, check your range of motion, and possibly perform a calf squeeze test or review an X-ray or MRI. Depending on the type and severity of your injury, your podiatrist may treat your condition with rest/ice/compression/elevation (RICE), nonsteroidal anti-inflammatory medications, heel lifts, and stretching and strengthening exercises. If you have torn your Achilles tendon, treatment may include physical therapy, ultrasound, shockwave therapy, or possibly even surgery.
Are Bunions Affecting Your Everyday Life?
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.








